Primary Care Toolkit
This toolkit has been developed through a collaboration between Thrive by Design and the University of Oxford Interdisciplinary Research in Health Sciences (IRIHS) team, as part of the NIHR funded ‘Remote by Default 2: The ‘new normal’’ research programme.
About this toolkit
-
This toolkit has been created for primary care practice teams, including clinical and non-clinical team members.
-
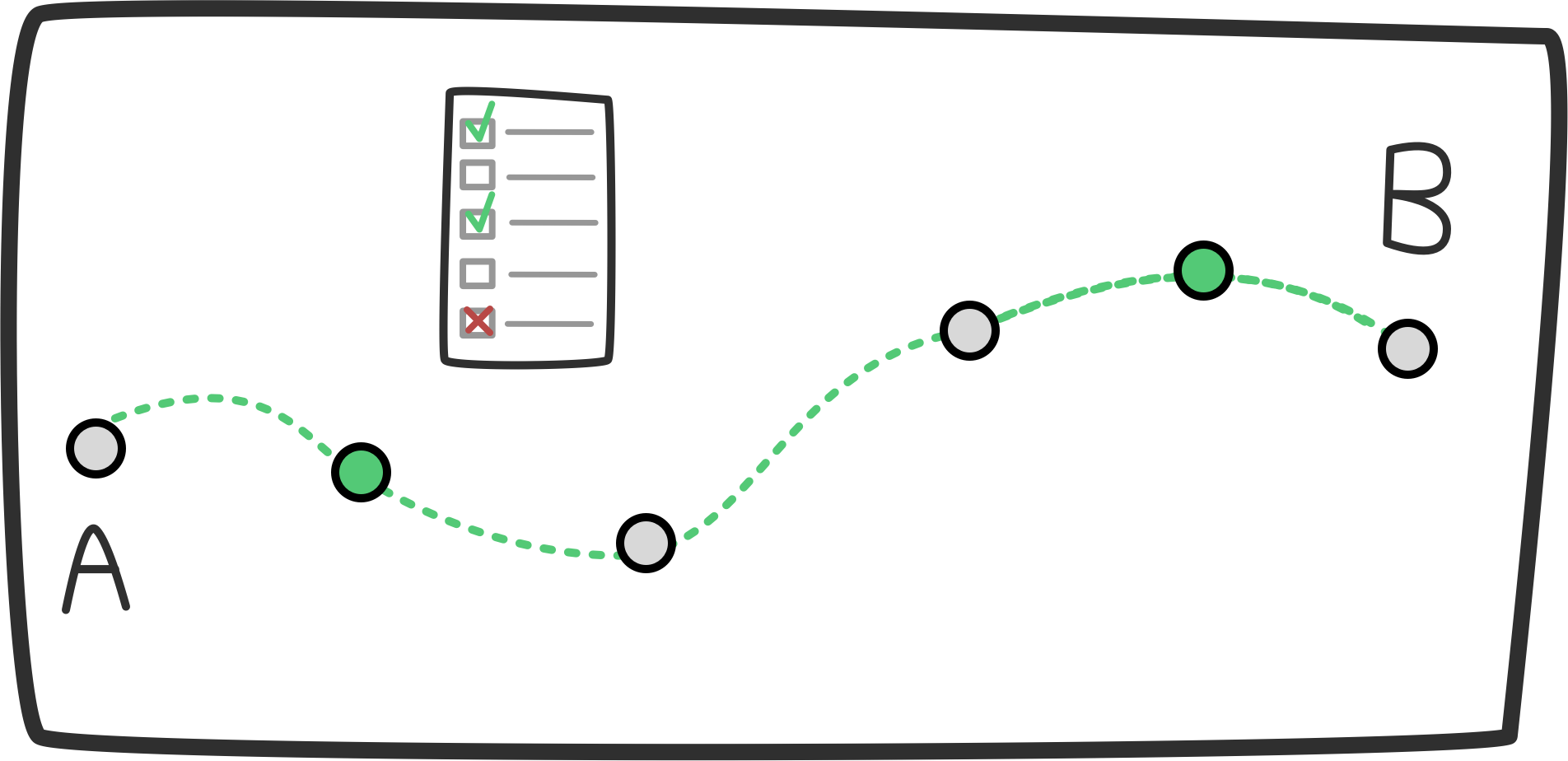
This toolkit provides activities that are based on design thinking methods. The activities are designed to support you to better understand your service from the point of view of those who use it, identify areas where you may be able to improve people’s experiences and then prioritise and test these ideas.
The overall goal is to support you on a collaborative and person-centred journey that results in a deeper understanding of how people experience your service and what might be done to make things equitable and more accessible for different people who use, or need to use, your service. You should be able to take away practical things you can try out and do within your setting.
These activities may be the first step in your journey, or they may help you to consolidate work you have done already. You can use the toolkit flexibly depending on your team’s needs.
-
This toolkit is based around a set of six activities that we would encourage you, where possible, to do with your team. The activities are provided below and can be downloaded as an activity pack.
For some of the activities you may need to refer to one or more of the guidance documents that make up this toolkit. This includes guidance on ‘journey mapping’, ‘accessibility and inclusion’ and ‘engagement’.
Activities
1: Understanding your service
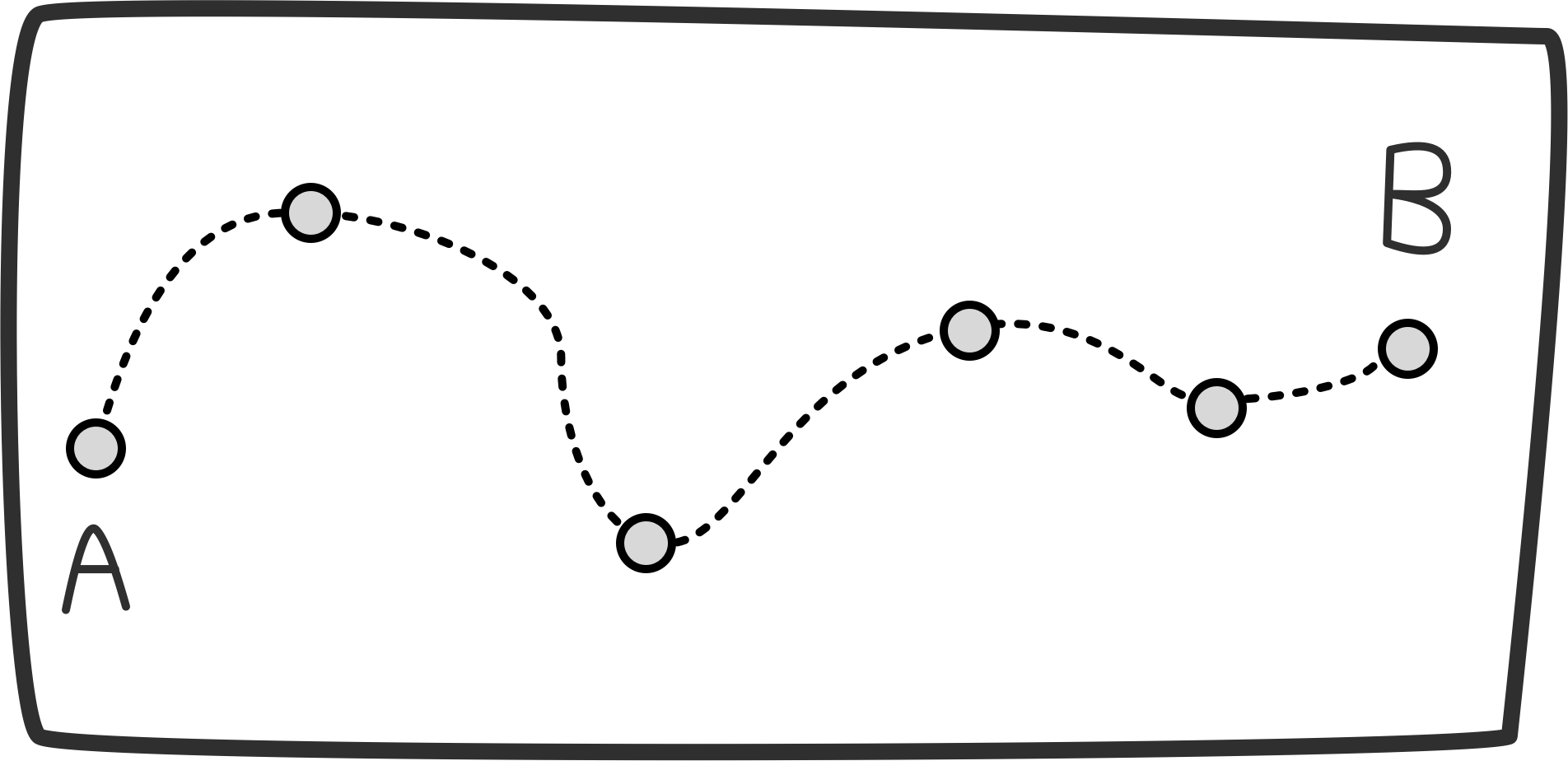
Understand and visualise the experience of service design and delivery from the perspective of different patients and their support networks, as well as the people who deliver your service.
Activity: use the journey mapping toolkit to support you to explore and visualise this with the different people impacted.
2: Channels and resources
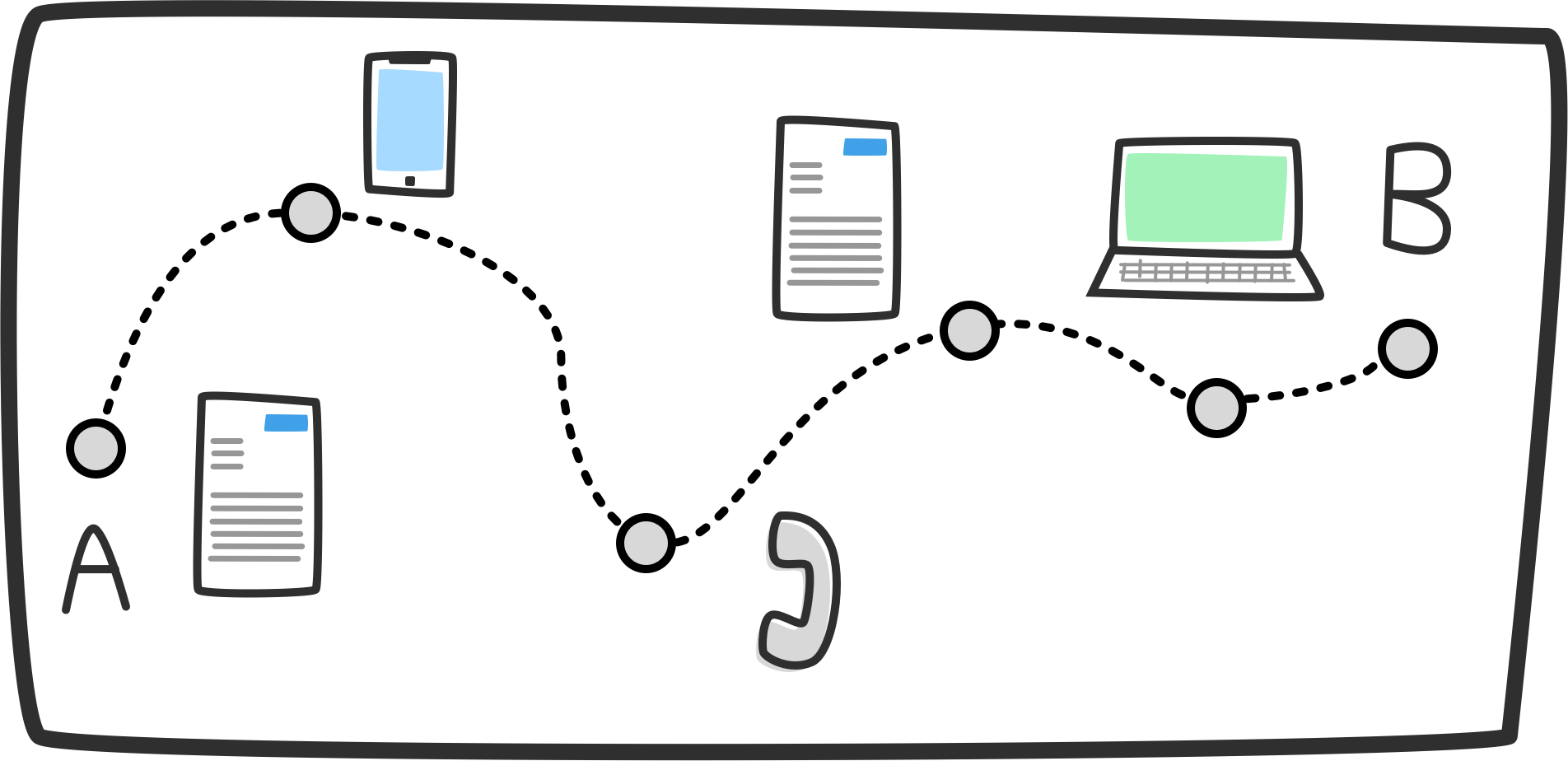
Understand what channels and resources are used to enable different interactions and communications in your service (including channels used to enable remote interactions).
This should consider:
Channels and resources that the GP surgery uses to deliver its service
Channels and resources that patients and their support networks must access and use to engage with the GP service (they may be in addition to, instead of, or a variation to what the service uses)
Activity: use the journey mapping toolkit to support you to explore and visualise this from different people's perspectives.
3: Barriers and challenges
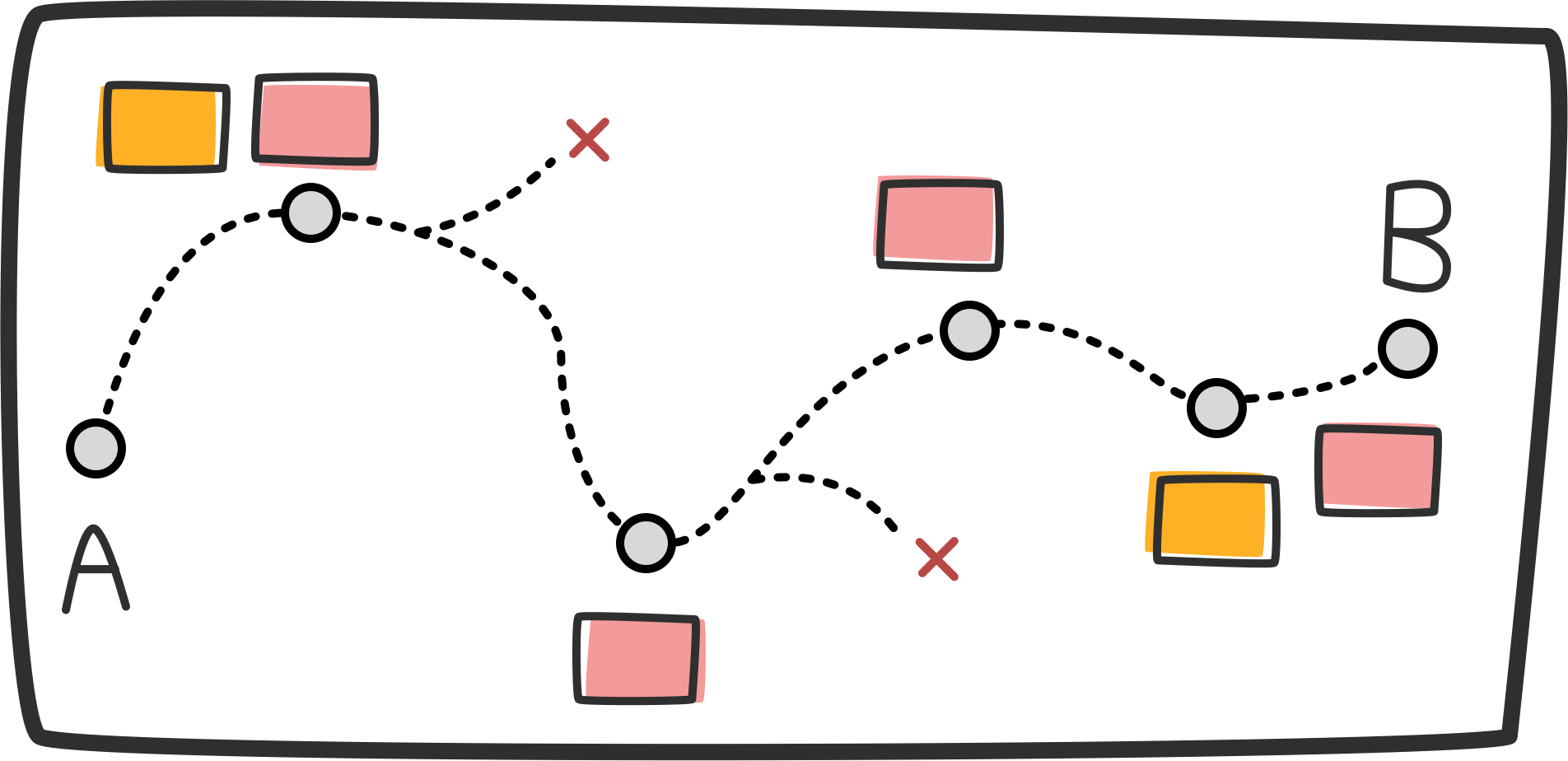
Understand the barriers and challenges that people experience when having to access and engage with:
Service design and delivery
Different channels and touchpoints
Activity: use the journey mapping toolkit to support you to explore and visualise this from different people's perspectives.
Key considerations:
At what point / stage in service delivery barriers are being experienced?
What tools or channels enable barriers?
Who experiences these barriers and why?
The cumulative impact and experience of these barriers for different people.
4: Opportunities for change
Activity: using the journey mapping toolkit and accessibility and inclusion guidance to guide you:
Evaluate how your current service delivery compares to the guidance, policy and legislation standards.
Highlight where changes or improvements can be made in relation to the opportunities, gaps or barriers you have visualised and documented.
Do this with your service staff and the people who use your service, as well as any other relevant stakeholders.
This could include: support organisations, VCSE organisations, other primary care stakeholders.
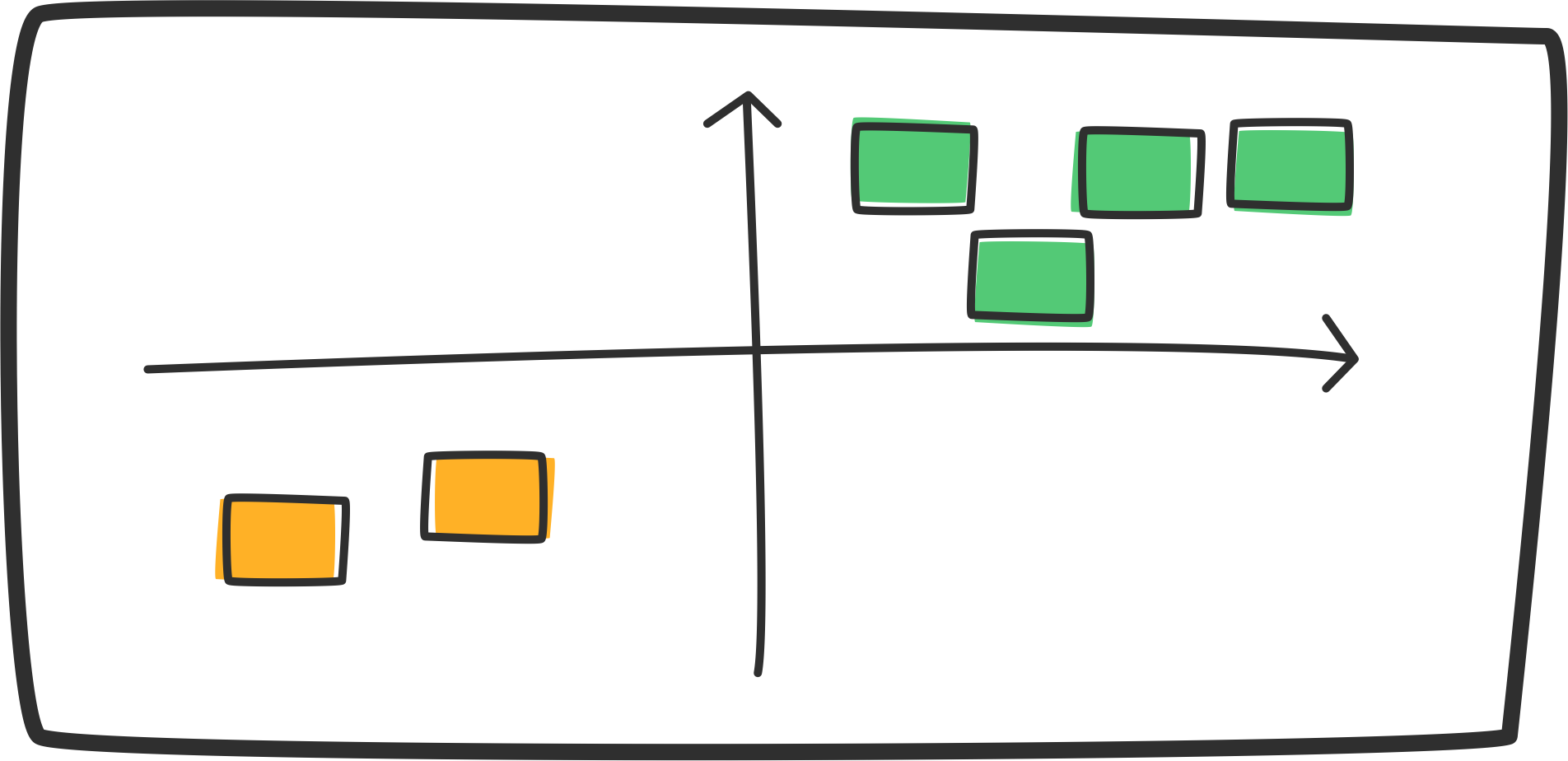
5: Prioritising change
Activity: Once you have explored your opportunities for change, prioritise your opportunities against the following considerations:
Organisational and service values.
Patient and support network (including carers) expectations and needs.
Current and future policy and legislation, examples of which can be found in the project accessibility and inclusion guidance.
Who may be experiencing the most barriers within your service.
Who may be at risk of experiencing barriers within your service.
Current and future funding.
Current and future service capacity.
Access to resources.
Access to support to make changes.
6: Prototyping and testing
Activity: Once you have an idea of your priority areas, create prototypes that will allow you to test out the changes that you have identified and prioritised. This might include the following steps:
Prototype any changes that need to be made.
Access support to do this, if needed.
Test the prototypes with different people.
Patients, their support networks, stakeholders and service staff.
Use engagement guidance for support.
Make this an iterative process and feedback loop.
Keep using the mapping activity to update your view of service design and delivery for different people, this will help you to orientate yourselves through any changes or service updates.
Share insights with your wider primary care networks to inform and refine your approach.
How this toolkit was developed
This toolkit has been developed through a collaboration between Thrive by Design and the University of Oxford Interdisciplinary Research in Health Sciences (IRIHS) team, as part of the NIHR funded ‘Remote by Default 2: The ‘new normal’’ research programme.
It is based on engagement work carried out by Thrive by Design in 2022-23 with and within primary care settings in England and Scotland. Conversations with patients, their support networks, healthcare professionals and different support staff helped us to build a picture of people’s experiences of accessing and engaging with GP services and primary care pathways.
Whilst this work was initially focussed on remote consultations, we understood from the engagement work completed that a remote consultation does not sit in isolation from other parts of someone’s journey within primary care. Therefore, this toolkit has been created to support primary care teams to explore their entire end-to-end service. Whilst this is the intention, teams are welcome to use the toolkit flexibly and adapt it to your local needs.
This toolkit is currently a prototype and we will be looking to iterate on and improve it with primary care teams over time.